
Dr. Ajay Narayan Sharma
Pediatric Hemato-oncologist & BMT Physician

Pediatric Hemato-oncologist & BMT Physician
Pediatric bone marrow transplant, also known as hematopoietic stem cell transplant, is a medical procedure that replaces damaged or diseased bone marrow with healthy stem cells from a donor. This treatment option is commonly used for children with certain cancers, primary immune deficiency diseases, and other conditions that affect the production of healthy blood cells. In this guide, we will explore the purpose, process, types, complications, and post-transplant care associated with pediatric bone marrow transplant.
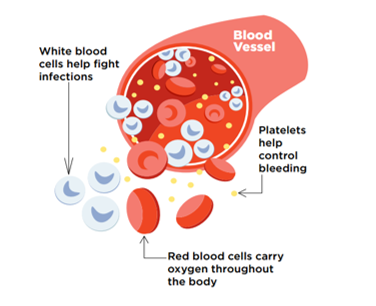
Restoring Hematopoietic Function: The primary goal of a bone marrow transplant is to restore the normal function of the patient's hematopoietic system, which includes the production of healthy red blood cells, white blood cells, and platelets. Treating Childhood Blood Cancers: Bone marrow transplants are commonly used in the treatment of childhood blood cancers such as leukemia, lymphoma, and myeloma.
Treating Primary Immune Deficiency Diseases: Bone marrow transplants are also an essential treatment option for children with primary immune deficiency diseases, which are genetic disorders that impair the immune system's ability to fight infections.
The donor can be a matched sibling, a family member, an unrelated donor, or cord blood from a public cord blood bank.
Prior to the transplant, the patient receives chemotherapy, radiation, or a combination of both to destroy the diseased cells and prepare the body to receive the donor cells.
The healthy donor stem cells are then infused into the patient's bloodstream, where they travel to the bone marrow and begin to produce healthy blood cells.
It takes a few weeks for the donor cells to establish themselves in the patient's bone marrow and start producing new blood cells.
The patient requires close monitoring, supportive care, and medications to prevent complications and manage side effects.